TMJ Gridding – Buxism
Temporomandibular Disorders (TMD)
Temporomandibular disorders (TMD) occur as a result of problems with the jaw, jaw joint and surrounding facial muscles that control chewing and moving the jaw. These disorders are often incorrectly called TMJ, which stands for temporomandibular joint.
What Is the Temporomandibular Joint (TMJ)?
The temporomandibular joint (TMJ) is the hinge joint that connects the lower jaw (mandible) to the temporal bone of the skull, which is immediately in front of the ear on each side of your head. The joints are flexible, allowing the jaw to move smoothly up and down and side to side and enabling you to talk, chew, and yawn. Muscles attached to and surrounding the jaw joint control the position and movement of the jaw.
What Causes TMD?
- Injury to the jaw, temporomandibular joint, or muscles of the head and neck.
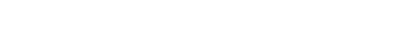
- Grinding or clenching the teeth, which puts a lot of pressure on the TMJ.
- Dislocation of the soft cushion or disc between the ball and socket.
- Presence of osteoarthritis or rheumatoid arthritis in the TMJ.
- Stress, which can cause a person to tighten facial and jaw muscles or clench the teeth.
What Are the Symptoms of TMD?
- Pain or tenderness in the face, jaw joint area, neck and shoulders, and in or around the ear when you chew, speak, or open your mouth wide.
- Limited ability to open the mouth very wide.
- Jaws that get “stuck” or “lock” in the open- or closed-mouth position.
- Clicking, popping, or grating sounds in the jaw joint when opening or closing the mouth (which may or may not be accompanied by pain) or chewing.
- A tired feeling in the face.
- Difficulty chewing or a sudden uncomfortable bite – as if the upper and lower teeth are not fitting together properly.
- Swelling on the side of the face.
- May occur on one or both sides of the face.
- Toothaches, headaches, neck aches, dizziness, earaches, hearing problems, upper shoulder pain, and ringing in the ears (tinnitis).
How Is TMD Diagnosed?
Because many other conditions can cause similar symptoms to TMD – including a toothache, sinus problems, arthritis, or gum disease – your dentist will conduct a careful patient history and physical examination to determine the cause of your symptoms.
Bruxism
Bruxism, or teeth grinding, is a common sleep disorder which can be caused by stress, some medications, a disturbed sleep pattern or lack of symmetry in the teeth.
Signs and symptoms
Most people who bruxism are unaware of the problem, either because there are no symptoms, or because the symptoms are not understood to be associated with a clenching and grinding problem. The symptoms of sleep bruxism are usually most intense immediately after waking, and then slowly get better, and the symptoms of a bruxing habit which occurs mainly while awake tend to slowly get worse throughout the day, and may not be present upon waking.[12] Bruxism may cause a variety of signs and symptoms, including:
- A grinding or tapping noise during sleep, sometimes detected by a partner or a parent. This noise can be surprisingly loud and unpleasant, and can wake a sleeping partner. Noises are rarely associated with awake bruxism.
- Cheek biting (which may manifest as and/or lineaalba), and/or lip biting, (other parafunctional activity which may occur together with bruxism).
- A burning sensation on the tongue (glossodynia), possibly related to a coexistent “tongue thrusting” parafunctional activity.
- Tenderness, pain or fatigue of the muscles of mastication,which may get worse during chewing or other jaw movement.
- Restricted mouth opening.
- Clicking of the temporomandibular joints.
- Headaches, particularly pain in the temples, (caused by muscle pain associated with the temporalis muscle).
- Inflammation of the periodontal ligament of teeth, which may make them sore to bite on, and possibly also a degree of loosening of the teeth.
- Pain or tenderness of the temporomandibular joints, which may manifest as preauricular pain (infront of the ear), or pain referred to the ear.
- Excessive tooth wear, particularly attrition, which flattens the occlusal (biting) surface.
- Tooth fractures, and repeated failure of dental restorations (fillings, crowns, etc.).
- Hypersensitive teeth, (e.g. dental pain when drinking a cold liquid) caused by wearing away of the thickness of insulating layers of dentin and enamel around the nerve.
- Indentations of the teeth in the tongue (“crenated tongue” or “scalloped tongue”).
- Hypertrophy of the muscles of mastication (increase in the size of the muscles that move the jaw), particularly the masseter muscle.
Causes
Psychosocial factors – Many studies have reported significant psychosocial risk factors for bruxism, particularly a stressful lifestyle, and this evidence is growing, but still not conclusive.
Some consider emotional stress to be the main triggering factor.
Genetic factors – Some research suggests that there may be a degree of inherited susceptibility to develop sleep bruxism.
Occlusalfactors – Inappropriate contacts between teeth,during biting and chewing. May cause bruxism.
Medication factors – Certain drugs, cause the development of bruxism, however others argue that there is insufficient evidence to draw such a conclusion.
Consequences
- Tooth wear
- Tooth mobility
- Pain
Management
- Repairing the damage to teeth Bruxism can cause significant tooth wear if it is severe, and sometimes dental restorations (crowns, fillings etc.) Some of these dental structures may be restored with crowns or whitefillings.
- Dental guards and occlusal splints It is an acrylic plate used mostly at night.
- Psychosocial interventions Given the strong association between awake bruxism and psychosocial factors. The relationship between sleep bruxism and psychosocial factors is unclear.
- Medication Many different medications have been used to treat bruxism, including benzodiazepines, anticonvulsants, beta blockers, dopamine agents, antidepressants, muscle relaxants, and others.
- Botox Botox injections are used in bruxism on the theory that a dilute solution of the toxin will partially paralyse the muscles and lessen their ability to forcefully clench and grind the jaw.
- Occlusal adjustment/reorganization Dentists will attempt to reorganize the occlusion in the belief that this may redistribute the forces and reduce the amount of damage inflicted on the dentition.